Submitted by Marcy Stevens Sauter IBCLC, PCD (DONA)
“Working with women on a daily basis, I have found that my story is not uncommon. Birthing women are very vulnerable, period. Most cultures are not sensitive to the needs of birthing women, especially here in North America where I reside.”
______________________________________
 On a recent trip to Bali, I attended a birth doula training that was taught by DONA trainer Debra Pascali-Bonaro. My intentions were not primarily geared to becoming certified, they were more to discover and attain birth healing for myself. After carrying a load of birth trauma for decades, my focus was to find peace for my heart and soul once and for all. The simplicity of being in the community of other women was very healing. Their non-judgmental company and listening ears made a huge impact on me. I needed the community of women to advance me on my journey.
On a recent trip to Bali, I attended a birth doula training that was taught by DONA trainer Debra Pascali-Bonaro. My intentions were not primarily geared to becoming certified, they were more to discover and attain birth healing for myself. After carrying a load of birth trauma for decades, my focus was to find peace for my heart and soul once and for all. The simplicity of being in the community of other women was very healing. Their non-judgmental company and listening ears made a huge impact on me. I needed the community of women to advance me on my journey.
Without going into the gory details of the traumas I experienced as a birthing woman, I have found that I am not alone in my quest for healing. Working with women on a daily basis, I have found that my story is not uncommon. Birthing women are very vulnerable, period. Most cultures are not sensitive to the needs of birthing women, especially here in North America where I reside.
Perhaps I was naive to think that I would be a hostess of the perfect birthing woman. My plan was to have my babies without any intervention. I imagined myself as a warrior woman whose body sustained life for 9 months to the growing baby and would continue to sustain him/her with my warm milk that my body produced. Far from it! With all four of my pregnancies, I think I had every intervention known to medical science. Despite successful breastfeeding, I still felt like a failure!
The good news here is this: there are women who experience great birthing outcomes. I’ve met them, I’ve worked with them! It gives me hope for future generations that birth will be esteemed, and it lights a fire under my feet to continue the work that I do as a postpartum doula, and IBCLC.
So what next? What will you do if you find yourself in a position like I have been in? A place where you find yourself with disappointment or depression due to unattained goals as a birthing woman.
Here’s my advice:
1. Find that community of women that will nurture you. Seek out the women in your community that are doulas, midwives, massage therapists, moms, grandmas, aunts, sisters, childbirth educators, lactation consultants, librarians, cashiers, WOMEN! There is so much we women can offer each other that is not tapped in to. Encompass yourself with the wisdom of other women, it can be healing.
2. Don’t wait for years on end to find healing! I waited for years, and the trauma manifested itself into depression and anxiety. Seek out mental health professionals that specialize in Post Trauma Stress Disorders. This step may help you avoid carrying around extra baggage of disappointment. It might be necessary, even with the community of women, to seek professional help. There are mental health issues that might need to be addressed that a specialized healthcare provider can treat.
3. Don’t blame your baby! If I was really honest with myself, at the time I gave birth, I would have to say that on a sub-conscience level, I put partial blame on my children as if they had something to do with the outcome. What a terrible load to put on an innocent baby! If you find yourself having difficulties in connecting with your infant, try wearing your baby and continue breastfeeding, which are instrumental for both baby and mama to heal the possible disconnect that the dyad may feel after having a difficult or disappointing birth.
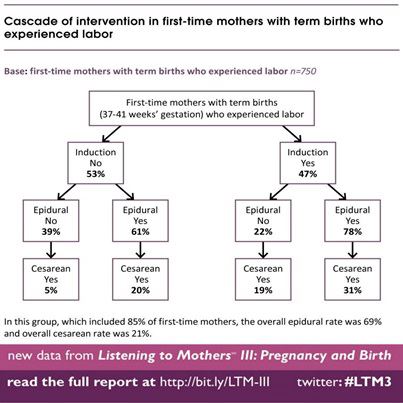
4. If you are pregnant, educate yourself about childbirth interventions, beforehand. I have observed that many women I’ve worked with, that have had positive birth outcomes are ones that opened themselves up to learn about the pros and cons of possible medical interventions.
In the event that you are hoping to have a non/low intervention birth, I recommend reading one or more of the following books:
Spiritual Midwifery by Ina May Gaskin
Gentle Birth Choices by Barbara Harper, Suzanne Arms
The Complete Book of Pregnancy and Childbirth (Revised) by Sheila Kitzinger
Ina May’s Guide to Childbirth by Ina May Gaskin
Misconceptions by Naomi Wolf
Orgasmic Birth Guide by Debra Pascali-Bonaro and Elizabeth Davis
And viewing the following videos/dvd’s:
Orgasmic Birth: The Best-Kept Secret
Business of Being Born
Birth Story: Ina May Gaskin and The Farm Midwives
In closing, it took me decades to finally leave a good portion of emotional turmoil, sustained by birth trauma, that I carried around for way too long.
I was privileged to attend two births of local Balinese women at Bumi Sehat, a birth Center in Ubud, where Robin Lim practices. These laboring moms were surrounded by the circle of women, which empowered them through their labor. I’ve decided to attend births as a birth doula a few times per year, here in the USA. In the meantime, I will use my skills and personal experience to help heal the hearts of women that have experienced birth trauma/disappointment.