 A Call for Birth Workers to have Breakfast in Bed with “Listening to Mothers III”
A Call for Birth Workers to have Breakfast in Bed with “Listening to Mothers III”
Submitted by Jill Wodnick, M.A., LCCE, ‘Giving Birth & Being Born’, Montclair State Univ. Center for Autism & Early Childhood Mental Health
It’s time for me to restock my Corn Flakes! Thanks to the support from the Kellogg Foundation, the Listening to Mothers III research was released May 9, 2013. In no surprise to birth professionals, a national survey of new mothers reveal that risky procedures in healthy populations are overused and many beneficial practices are underused. My hope is that the leverage of this report found in today’s Wall Street Journal and Consumers Reports is that the conversation will expand and permeate into the paradigm of optimal maternity care.
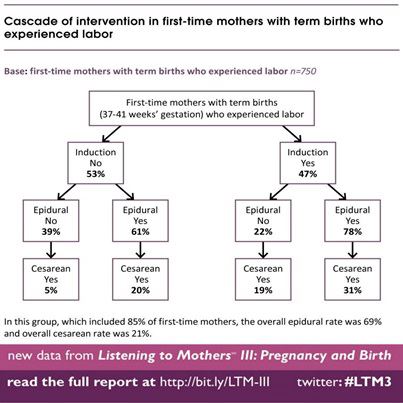 In a tale of two labors, inductions had drastic birth outcome implications. 53% of women had inductions; whereas 47% had no induction. Looking at birth outcomes, the woman who went into labor without an induction and without an epidural had a cesarean birth rate of 5%; the woman who had an induction and epidural had a cesarean birth rate at 31%. The value of the Listening to Mothers is that Childbirth Connection did just that: listened with clarity over the past decade to mothers from all over America making a real imprint in the buzz word of ‘patient centered care.’
In a tale of two labors, inductions had drastic birth outcome implications. 53% of women had inductions; whereas 47% had no induction. Looking at birth outcomes, the woman who went into labor without an induction and without an epidural had a cesarean birth rate of 5%; the woman who had an induction and epidural had a cesarean birth rate at 31%. The value of the Listening to Mothers is that Childbirth Connection did just that: listened with clarity over the past decade to mothers from all over America making a real imprint in the buzz word of ‘patient centered care.’
Today’s webinar by Childbirth Connection to present the Listening to Mothers III featured a cross section of change makers. In hearing Leah Binder, president of the Leap Frog Group focus on the employers and purchasers of health care, she was quick to point out that labor and delivery make-up 25% of hospital charges. New Jersey’s own Dr. Thomas Westover, M.D., Co-Chair, New Jersey Hospital Association Perinatal Safety Collaborative, Assistant Professor, Maternal & Fetal Medicine & OB&GYN, Robert Wood Johnson Medical and Cooper Medical School detailed the need to engage payers so hospitals have the capacity offer consistent VBAC access.
Aligning incentives for higher quality care will go a long way to foster the gap that is in maternity care between protocols and best practices. Only 2 out of 5 women walked around during labor. More than two-thirds (68%) of women who gave birth vaginally reported that they lay on their backs while pushing their baby out and giving birth. The anonymous quotation of this woman tells the journey of what so many women experience: “I was not allowed to get up and walk around, even go to the restroom, after I had been strapped with the fetal monitor.”
The fact that freedom of movement is not consistently accessible nor available begins the cascade of many interventions which drive up cost and can derail the treatment of women. Issues of equity, access and disparities all make this report critical to review.
Callers on the webinar about Listening to Mothers III asked about sharing this information with medical providers and the challenge for employers to support education and information for pregnant women.
Third times a charm. The last two LTM surveys have been a much needed voice in patient centered care and narrative medicine. Now, we have a decade worth of Listening to Mothers. We can list out the need to improve care and the list of underused comfort measure and list over used procedures. We can find that in the past decade, our lists may have gone on deaf ears when it comes to consistent implementation of best practices.
The root word of both list and listen is the Indo European word root of kleu. They are together because listening involves tilting or leaning over to a side to hear something. So hear the direct words of LTM III:
‘Over the three Listening to Mothers surveys, respondents have increasingly supported the idea that birth processes should not be interfered with unless medically necessary. However, there was little indication that the maternity care system protects, promotes, and supports the intrinsic physiologic capacities of this largely healthy population of women and their fetuses/newborns.
Technology-intensive maternity care continues to predominate.
Our maternity care system is failing to provide care that many mothers told us they want and that is in the best interest of themselves and their babies. Moreover, this unnecessarily costly style of care places a considerable burden on governments, employers, and families who pay the bills for this major sector of the health care system.
The Institute of Medicine’s landmark Crossing the Quality Chasm report exposed the gulf between where our health care system is and where it should be with respect to safety, effectiveness, patient-centeredness, timeliness, efficiency, and equity.’
As you take the time to read Listening to Mothers III, take a moment over your own breakfast cereal to read the research. You will digest the research and resources of what maternity care can be in the United States and our role in the many dimensions of care.
 Jill Wodnick teaches didactic sessions to medical residents as well as Lamaze Childbirth Education through Montclair State University’s Center for Autism & Early Childhood Mental Health. Speaking frequently about birth, she recently delivered a webinar for the NJ Hospital Association on sustaining NJ’s BabyFriendly Hospital Initiative through the use of doulas. She can be found singing and playing board games with the 3 boys and husband in Montclair, NJ. www.JillWodnick.com
Jill Wodnick teaches didactic sessions to medical residents as well as Lamaze Childbirth Education through Montclair State University’s Center for Autism & Early Childhood Mental Health. Speaking frequently about birth, she recently delivered a webinar for the NJ Hospital Association on sustaining NJ’s BabyFriendly Hospital Initiative through the use of doulas. She can be found singing and playing board games with the 3 boys and husband in Montclair, NJ. www.JillWodnick.com
Leave a Reply