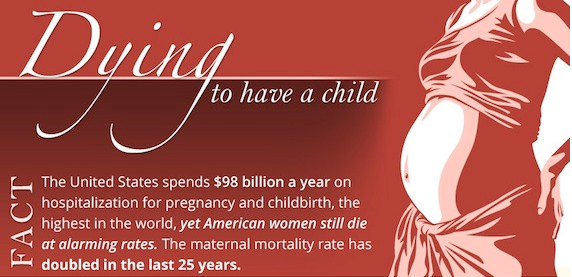
While in Malaysia this past week speaking about respectful care, I always love the opportunity to open up the topic of pleasure, ecstasy and Orgasmic Birth. It is too often a forgotten aspect of childbirth, or the one aspect that is avoided, as to talk about pleasure and/or the sexuality of birth can make many people uncomfortable. Yet, for me it is an essential topic if we are to look at the ways to honor, respect and offer women the options and care that will make childbirth as safe and easy as possible. To only talk about birth in our current medical, technocratic paradigm of pain and fear is to miss key elements that can transform childbirth and a woman’s experience of pain into pleasure, bliss and joy.
At the closing panel for Women Deliver, Kavita N Ramdas (Ford Foundation representative in New Delhi serving India, Nepal and Sri Lanka) gave a wonderful presentation summing up all the topics 4500 people from 159 countries had come together to discuss and brought up how we need to talk about pleasure too. I smiled, as I could not agree more. In addition this week Science Direct published Childbirth Climax: The Revealing of Obstetrical Orgasm stating, “Some mothers report experiencing intense physical pleasure during childbirth, which conflicts with popular belief and cultural taboos.” The author surveyed midwives; “the survey showed that 85% of the midwives questioned knew that it was possible to experience physical pleasure during childbirth. Nevertheless, 31% of respondents never observed a case, while 99% of the cases reported were observed by only 50% of the midwives questioned.”
Sitting in my hotel lobby in Kuala Lumpur, I was interviewed by Stephanie Pappas for my comments on the new study. I shared how many women have told me they never told anyone, including their partners, that birth was pleasurable as they felt ashamed that something our culture tells us should be only painful can be pleasurable. So, when asking caregivers how often they see pleasurable birth, I am not sure they always know what the women are feeling. Would you feel you need to share with your doctor or midwife if you had a pleasurable or orgasmic birth?
I am so grateful to the author of the study T. Postel, who adds another layer of information to open up our minds to all that birth can hold. In the conclusion: “by producing proof that a mother can experience physical pleasure during childbirth, this study constitutes an additional element in the understanding of the already- polymorphous female orgasmic response, and calls the function of orgasm back into question (Reich, 1986). It sheds new light on birthing conditions, midwife education, and labor preparation (Van Der Schueren, 2003).”
It is time we acknowledge scientifically the ability to find pleasure in childbirth. In addition, as T. Postel suggest we must look at the birth environment or as I call birth ambiance, we must include training on the natural physiology and the hormones of childbirth that can lead to pleasure in education for our midwives, nurses and physicians. As well as, we must provide education and offer preparation for women and men so that we recognize the connection between pain and pleasure and help women find the path to a safe, satisfying and pleasurable birth. As the article states, and I could not agree more, Orgasmic Birth should not be a performance standard, yet we should honor the potential for birth to be pleasurable and offer the options, environment and respectful care that optimizes the possibilities. I believe we must address why many people feel more comfortable with birth as painful and the mention of birth with pleasure as controversial.
Please share your thoughts and comments with me on this blog, the study, and the follow up article. To read Stephanie’s follow up article please visit: http://www.livescience.com/37039-orgasmic-birth-real.html.
I continue to collect women’s stories and comment and as I am preparing a webinar series, article and more on pleasurable birth, I hope to hear from you!
Pleasurably Yours,
Debra